Stand up for the facts!
Our only agenda is to publish the truth so you can be an informed participant in democracy.
We need your help.
I would like to contribute
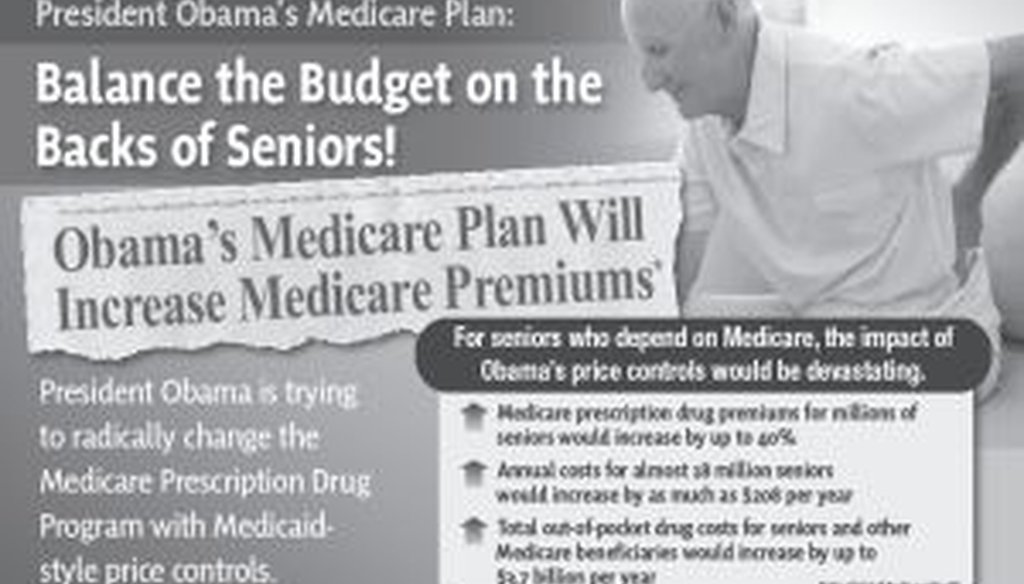
A representation of the mailer distributed by American Action Network in 32 Congressional districts.
The national debate over changes to the Medicare prescription drug program has hit mailboxes
in two of New Jersey’s Congressional districts.
American Action Network, a conservative advocacy group, sent out mailers earlier this month criticizing a Democratic proposal to force drug manufacturers to pay higher rebates under the Medicare Part D program.
Due to those higher rebates, Medicare premiums would increase by up to 40 percent, according to American Action Network.
"Obama’s Medicare Plan Will Increase Medicare Premiums" the mailers’ read. "For seniors who depend on Medicare, the impact of Obama’s price controls would be devastating."
The mailers were distributed to residents in 32 Republican-controlled Congressional districts across the country, including those of New Jersey congressmen Leonard Lance and Jon Runyan.
A couple of readers asked PolitiFact New Jersey to submit the Lance mailer to the Truth-O-Meter to determine its accuracy. However, we cannot do that, because the mailer is making a prediction based on a set of assumptions. We can only check facts.
First, let’s explain how we arrived at this current debate.
Before Medicare Part D was set up in 2006, individuals who are dually eligible for benefits under Medicaid and Medicare received their prescription drug coverage through Medicaid. Under Medicaid, drug companies are required to pay rebates to state Medicaid agencies for the use of their products.
As defined by federal law, those rebate amounts represent a percentage of the average price that manufacturers receive for sales to retail pharmacies.
In 2006, dual-eligible individuals were shifted into Medicare Part D and the federal government began contracting with private insurance companies to provide drug coverage for them and other Medicare Part D enrollees. But a major change also occurred when it comes to the rebates received for drugs used by dual-eligible individuals.
Unlike under Medicaid, manufacturers no longer had to pay minimum rebate amounts for Medicare Part D. Instead, manufacturers negotiate rebates with the private insurance companies.
Based on those discounted prices, private insurance companies may pass the savings on to consumers in two ways: by reducing premiums or by reducing prices that consumers pay when they purchase drugs.
The federal government pays 75 percent of premiums for most enrollees, who are responsible for the remaining 25 percent. The government kicks in more money for dual-eligible and other individuals in the Low-Income-Subsidy program.
However, because there is no statutory requirement on rebates in Medicare Part D, those rebates have been lower than under Medicaid.
Now, let’s talk about the proposed changes at the center of American Action Network’s campaign.
The target of the mailers is the Medicare Drug Savings Act of 2011 -- proposed legislation aimed at requiring manufacturers to pay rebates for drugs used by Low-Income-Subsidy individuals similar to those required under Medicaid.
Under the legislation, manufacturers would have to pay the difference between the average rebates currently paid to insurance companies and 23.1 percent of the Average Manufacture Price, which is the price received for sales to retail pharmacies. That difference would be paid to the federal government.
If drug prices increase faster than the inflation rate, manufacturers would have to pay additional rebates to the federal government.
The Congressional Budget Office has said such a proposal would amount to about $112 billion to the federal government between 2012 and 2021. But the budget office also said the move would lead to a reduction in the privately negotiated rebates.
American Action Network takes that projection one step further. According to the group, the higher rebate could lead to a reduction in existing rebates paid to insurance companies. As a result, premiums could rise for Medicare Part D consumers, according to the group.
An analysis done by its sister organization, American Action Forum, is cited in the mailers as the basis for this argument.
"If the government imposes its own mandatory rebates and the market responds in ways that reduce privately negotiated rebates (as CBO has suggested it will), the impact could be significant," according to that analysis.
A 2009 report commissioned by the Pharmaceutical Research and Manufacturers of America also said a Medicaid-style rebate would impact the non-dual eligible population in Medicare Part D. That group could see its monthly premiums increase by between roughly 25 and 50 percent, according to the report.
But the group’s argument still raises some questions. According to a few experts, American Action Network may be overstating the impact of the proposed rebates on Medicare premiums.
Jack Hoadley, a health policy analyst with Georgetown University's Health Policy Institute, pointed out how the government pays a substantial share of Part D premiums. Given the CBO’s projected savings, Hoadley suggested the budget office doesn't find a large premium increase, if any, likely, Hoadley said in a series of emails.
"I'm skeptical of their claims since it seems to me like they are giving modest changes in rebates too much leverage on the premiums," Hoadley said. "But even if there was some reduction in rebate income (for insurance companies), the rebate income is just one piece of their revenues and thus just one factor in determining their premium bids."
Gerard Anderson, director of the Center for Hospital Finance and Management at Johns Hopkins University, has argued that the proposal would lead to lower prices paid to drug companies and lower costs to Medicare beneficiaries.
"My expectation based on my analysis of the Medicaid rebate program is that expanding the rebate to include dual eligibles and low income individuals will lower the out of pocket costs and premiums for all Medicare enrollees," Anderson wrote in a letter to Congressman Henry Waxman, the sponsor of the bill.
Anderson added, "The assumption that drug companies can cost shift to Part D plans assumes that the Part D plans are not price sensitive and unable to negotiate effectively with the drug companies."
Rutgers University professor Stephen Crystal suggested American Action Network has not made a convincing argument that the higher rebate would lead to higher premiums.
Crystal noted in an email, "Once a drug is approved, the actual cost of producing an additional unit of the drug is very small relative to even the most heavily discounted prices that are paid."
Where does all this leave us?
PolitiFact New Jersey is not issuing a Truth-O-Meter ruling on American Action Network’s claim because it’s a prediction. But as you can see, the impact of a higher rebate on Medicare premiums remains subject to debate.
A study commissioned by the pharmaceutical research industry supports the group’s claim, but some experts have said the argument may be overblown.
To comment on this story, go to NJ.com.
Our Sources
American Action Network, mailers sent to 32 Congressional districts, accessed Aug. 16, 2011
Phone and email interviews with Jim Landry, American Action Network, Aug. 16, 2011
American Action Forum, Cost Shifting Debt Reduction to America’s Seniors, July 21, 2011
House Committee on Energy and Commerce, House Democratic Leaders Introduce Legislation To Save More Than $100 Billion In Medicare Drug Costs, June 16, 2011
Congressional Budget Office, Reducing The Deficit: Spending and Revenue Options, March 2011
U.S. Department of Health and Human Services Office of Inspector General, Higher Rebates for Brand-Name Drugs Result in Lower Costs for Medicaid Compared to Medicare Part D, Aug. 15, 2011
House Committee on Oversight and Government Reform, Medicare Part D: Drug Pricing And Manufacturer Windfalls, July 2008
Email interviews with Jack Hoadley, Georgetown University Health Policy Institute, Aug. 17 and 24, 2011
New York Times, Waxman Takes on Drug Makers Over Medicare, Aug. 25, 2009
Ingenix Consulting and The Lewin Group, Financial Impacts on Medicare Beneficiaries if Larger Part D Rebates Are Required for Medicare/Medicaid Dual Eligibles, June 25, 2009
H.R. 2190, the Medicare Drugs Savings Act, Saves $120 Billion While Reducing Part D Drug Costs and Premiums for Seniors, letter sent by U.S. Reps. Henry Waxman and Pete Stark, July 28, 2011
Letter to U.S. Rep. Henry Waxman from Gerard Anderson, John Hopkins Center for Hospital Finance and Management, July 28, 2011
The Henry J. Kaiser Family Foundation, The Medicare Part D Low-Income Subsidy Program: Experience To Date and Policy Issues for Consideration, September 2010
U.S. Department of Health and Human Services Office of Inspector General, Concerns With Rebates In The Medicare Part D Program,March 2011
Phone and email interviews with Stephen Crystal, Rutgers University Institute for Health, Health Care Policy and Aging Research and the School of Social Work, Aug. 25-26, 2011
Email interview with Karen Lightfoot, House Committee on Energy & Commerce, Aug. 26, 2011