Get PolitiFact in your inbox.
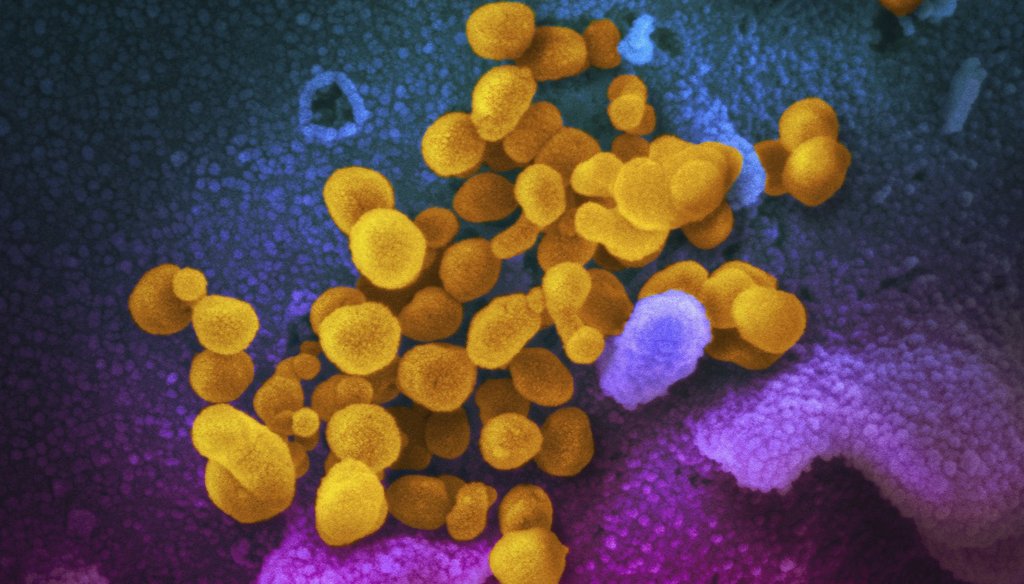
This undated electron microscope image made available by the U.S. National Institutes of Health in February 2020 shows the Novel Coronavirus SARS-CoV-2, yellow, emerging from the surface of cells, blue/pink, cultured in the lab. (NIAID-RML via AP)
If Your Time is short
- Before the Affordable Care Act, health insurers could look at a person's medical history and determine coverage options. People with pre-existing conditions could have less access to care or could be charged more for it.
- This practice affected people shopping for insurance on the individual market.
- The ACA, also known as Obamacare, is the subject of a U.S. Supreme Court case, to be heard in November. Provisions of the law, or the whole thing, could be struck down.
- COVID-19 could be considered a pre-existing condition, experts said, based on what they know of insurers' behavior prior to the ACA.
- In New York, there are protections for people with pre-existing conditions, in addition to those contained in the ACA.
Democrats have been talking about the Republican-led legal challenge to the Affordable Health Care Act and how that could affect costs and coverage for people with health problems.
In a Facebook post on Sept. 23, Rep. Tom Suozzi, a Democrat from Long Island, wrote: "It is inconceivable that in the midst of a global pandemic that has affected more than 6 million Americans, the Trump administration is still in court trying to take away protections for those with pre-existing conditions. Take note, that anyone in this country who has had COVID, or ever tests positive for the COVID antibodies, has a pre-existing condition."
We’ve heard this claim from other Democrats, and we wondered whether everyone who has been diagnosed with the novel coronavirus, or has COVID-19 antibodies, has a pre-existing condition for the purposes of health insurance coverage.
Coming hearing
The challenge to the Affordable Care Act, also known as Obamacare, is scheduled to be heard by the U.S. Supreme Court after the presidential election, on Nov. 10. The court’s decision could spell the end of the health care law, a possibility that has been emphasized by Democrats since the death of Justice Ruth Bader Ginsburg, a liberal icon.
The challenge concerns the individual mandate, or the requirement that people carry a minimum amount of coverage. The lawsuit, however, could put all of it or other major provisions of the law in jeopardy, including protections for people with pre-existing conditions. If the ACA’s provision protecting people with pre-existing conditions is struck down, the matter could be left up to each state, according to an analysis of the case from the nonpartisan Kaiser Family Foundation.
Before Obamacare, there was no broad federal law protecting people from being discriminated against when they tried to purchase health insurance on the individual market because of health conditions they may have. Pre-existing conditions used by insurers to make coverage decisions in the past included epilepsy, lupus, HIV/AIDS, and rheumatoid arthritis, according to the Kaiser Family Foundation. In New York, however, there are protections for people with pre-existing conditions, regardless of whether the ACA is struck down by the high court.
COVID as pre-existing condition
We spoke with six health care policy experts about whether a COVID diagnosis or the presence of COVID antibodies would be considered a pre-existing condition if the ACA was struck down. Most agreed that insurers would consider it a pre-existing condition. They said that insurers don’t like uncertainty, and the virus’s possible long-term effects aren’t fully known, which increases the likelihood that it would be considered a pre-existing condition.
Sherry Glied, a health economist who has worked in Republican and Democratic presidential administrations, said that there is no set list of pre-existing conditions, and that before the ACA, in general, health insurers could determine what they wanted to consider a pre-existing condition. Based on past practice, it’s likely COVID would be on their list, though the government could step in to bar this practice, she said.
"I would expect insurance companies to consider anyone testing positive for COVID-19, regardless of whether they experienced symptoms, to have a ‘pre-existing condition,’" said Sabrina Corlette, a research professor, founder, and co-director of the Center on Health Insurance Reforms at Georgetown University’s McCourt School of Public Policy. "That could change down the road if we learn that there are no long-term effects from having COVID, but we don't know that," and therefore Suozzi’s statement is accurate, she said.
Katherine Hempstead, a senior policy advisor at the Robert Wood Johnson Foundation, said insurers "could certainly decide" to add COVID-19 to their lists of pre-existing medical conditions for the purpose of making coverage decisions.
"There is mounting evidence that some people have significant long-term effects including cardiovascular damage from COVID, which could be a reason why insurers would want to exclude them," she said.
Karen Pollitz, a senior fellow at the Kaiser Family Foundation, has studied medical underwriting in the individual market and said based on past practice, "I would say that COVID-19 definitely could be considered a pre-existing condition under private health insurance if the ACA protections were to be overturned."
Another expert, Thomas P. Miller, a health economist and lawyer who co-wrote "Why Obamacare is Wrong for America," noted that people in employer-based plans have protections from other federal laws, and that if the ACA is struck down, states could regulate pre-existing conditions.
Larry Levitt, executive vice president for health policy at the Kaiser Family Foundation, said that he is not aware of any health insurance company that has said that they would add COVID-19 to their list of pre-existing conditions if the ACA were overturned. "But, I do think it’s very likely insurers would deny coverage, charge higher premiums, or limit benefits for people who have recently had COVID-19," Levitt said.
We asked a large health insurance advocacy group, America’s Health Insurance Plans, whether COVID would be considered a pre-existing condition. Spokeswoman Kristine Grow said that "our focus is on protecting people with pre-existing conditions, not determining what new pre-existing conditions would be." The group has filed a brief with the U.S. Supreme Court in support of the ACA.
We also reached out to Suozzi’s spokesperson, Dylan Smith, who sent us articles and a study about the long-term effects of the novel coronavirus found in some patients, such as heart inflammation and issues in the brain.
On Sept. 23, Dr. Anthony Fauci testified in Congress about coronavirus patients who experience health troubles such as fatigue, fever, brain and heart problems after they have recovered from the infection.
In July, Kaiser Health News, a PolitiFact partner, fact-checked a claim from Democratic presidential nominee Joseph Biden: "If Donald Trump has his way, complications from COVID-19 could become a new pre-existing condition." KHN found it to be Mostly True.
President Donald Trump signed an executive order on Sept. 24 that he says protects people with pre-existing conditions, though PolitiFact reporting shows that if the ACA is struck down, more action is needed by the federal government to truly protect people with pre-existing conditions from limited coverage or higher prices.
No ruling
Suozzi claimed that a person who gets COVID-19 or tests positive for COVID-19 antibodies, "has a pre-existing condition." We aren't making a ruling in this case because Suozzi is making a claim about circumstances that haven't happened yet. (Suozzi’s statement, unlike the Biden claim that Kaiser Health News fact-checked, did not come couched with the phrase "could become a new pre-existing condition.")
We know from past practice that health insurers used information in a person’s health history to limit coverage or charge more for it.
If the ACA is struck down, in the absence of other federal or state actions, it’s likely that insurers could consider a person's history with COVID-19 as a pre-existing condition when offering insurance on the individual market.
Our Sources
Facebook post, Rep. Tom Suozzi, Sept. 23, 2020. Accessed Sept. 23, 2020.
Kaiser Family Foundation, health brief, "Explaining California v. Texas: A Guide to the Case Challenging the ACA," Sept. 1, 2020. Accessed Sept. 29, 2020.
The Commonwealth Fund, To the Point blog, "Lawsuit Threatens Affordable Care Act Preexisting Condition Protections But Impact Will Depend on Where You Live," Aug. 29, 2018. Accessed Sept. 29, 2020.
PolitiFact, "Republican pre-existing protections leave some vulnerable," April 1, 2019. Accessed Sept. 29, 2020.
Kaiser Health News/PolitiFact, "Could Trump’s Push To Undo The ACA Cause Problems For COVID Survivors? Biden Thinks So," July 9, 2020. Accessed Sept. 23, 2020.
Washington Post, analysis, "The Health 202: Coronavirus could be considered a preexisting condition if Obamacare is struck down," Sept. 22, 2020. Accessed Sept. 23, 2020.
Axios, article, "If Trump replaces Ginsburg, the ACA really is at risk," Sept. 21, 2020. Accessed Sept. 23, 2020.
Kaiser Family Foundation, "Pre-Existing Condition Prevalence for Individuals and Families," Oct. 4, 2019. Accessed Sept. 30, 2020.
Email interview, Dylan Smith, spokesperson, Rep. Tom Suozzi, Sept. 24, 2020.
Journal of American Medicine Cardiology, Research Letter, "Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection," Saurabh Rajpal, Matthew S. Tong, James Borchers, et. al., Sept. 11, 2020. Accessed Sept. 30, 2020.
New York Times, article, "How the Coronavirus Attacks the Brain," Sept. 9, 2020. Accessed Sept. 30, 2020.
Email interview, Kristine Grow, senior vice president of communications, America’s Health Insurance Plans, Sept. 28, 2020.
Phone Interview, Thomas P. Miller, resident fellow, American Enterprise Institute, Sept. 28, 2020.
Phone interview, Sherry Glied, dean, NYU Wagner School of Public Service, Sept. 29, 2020.
Email interview, Karen Pollitz, senior fellow, health reform and private insurance, Kaiser Family Foundation, Sept. 28, 2020.
Email interview, Larry Levitt, executive vice president for health policy, Kaiser Family Foundation, Sept. 28, 2020.
Email interview, Sabrina Corlette, research professor, Center on Health Insurance Reforms, Georgetown University McCourt School of Public Policy, Sept. 28, 2020.
Email interview, Katherine Hempstead, senior policy adviser, Robert Wood Johnson Foundation, Sept. 29, 2020.
Factcheck.org, "Biden Misleads on Preexisting Conditions," Sept. 1, 2020. Accessed Sept. 30, 2020.
Rev.com, transcript, "Fauci, Redfield COVID-19 Senate Testimony Transcript September 23," Sept. 23, 2020. Accessed Sept. 30, 2020.
PolitiFact, "Donald Trump’s executive order on preexisting conditions lacks teeth, experts say," Sept. 25, 2020. Accessed Oct. 2, 2020.