slide 1 of 1
Improve Obamacare
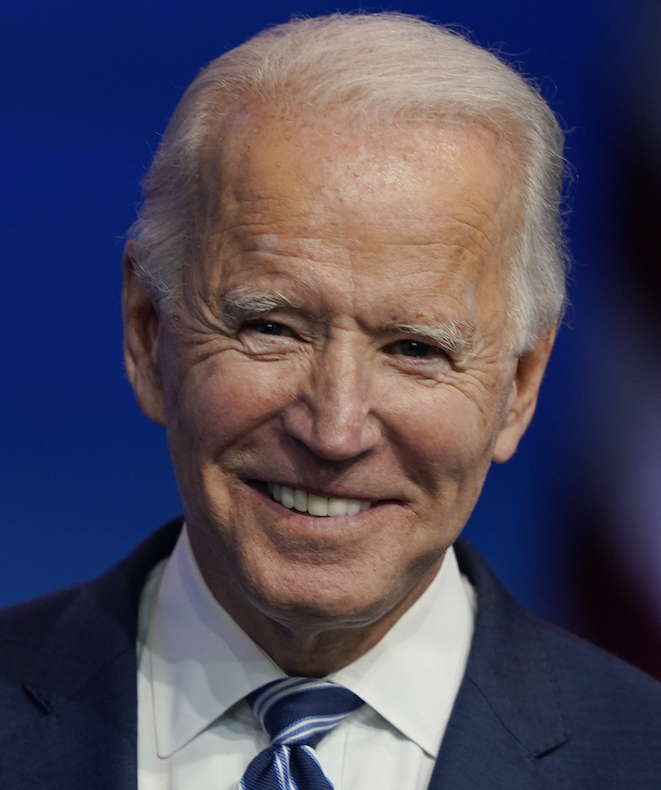
Joe Biden
"I’ll not only restore Obamacare, I’ll build on it."
Biden Promise Tracker
Promise Kept
Our only agenda is to publish the truth so you can be an informed participant in democracy.
We need your help.
In a Nov. 2, 2020 speech, then-presidential candidate Joe Biden promised, "I'll not only restore Obamacare; I'll build on it."
Two years and counting since then, how is he doing in meeting that promise?
Eight days into his tenure as president, Biden signed an executive order aimed at strengthening Medicaid and the Affordable Care Act, or Obamacare. A couple of months later, he signed his first major piece of legislation, the American Rescue Plan, which included provisions expanding eligibility for subsidies and increasing premium tax credits available to help low- and moderate-income Americans purchase ACA coverage.
That legislation also offered financial incentives to encourage the 12 states that had declined to expand Medicaid eligibility to do so.
Those subsidies for consumers were originally set to expire in 2023 but were extended by the Inflation Reduction Act, which Biden signed into law Aug. 16, after much debate and without any Republican votes. The measure also continued the expanded eligibility for subsidies.
In October, the Biden administration addressed another issue in the ACA, the "family glitch," which prevented some people with job-based insurance from qualifying for subsidies.
Those items alone prompt "an unequivocal yes," to the question of whether Biden has met his campaign promise, said Sabrina Corlette, co-director of the Center on Health Insurance Reforms at Georgetown University.
Joe Antos, a senior fellow at the American Enterprise Institute think tank, offered a different perspective — that the actions taken on the glitch can't count toward Biden's promise to "restore" the ACA. Antos said that's because it wasn't a glitch at all, but an intentional element of the original ACA, put there to save the government money, and help win its passage in Congress.
"Biden was vice president when the bill was signed into law, and he supposedly supported it," Antos said.
Corlette touted other Biden administration changes, including increased funding for consumer assistance programs that help people sign up for ACA coverage and streamlined some of the paperwork required for enrollment.
The White House issued an official recap of other actions stemming from the executive order, including extending the annual open enrollment period to bring in more policyholders, and allowing low-income Americans to sign up anytime.
Last year, a record 14.5 million Americans selected an ACA plan. This year's open enrollment closed Jan. 15 in most places and, based on preliminary numbers, enrollment in 2023 will continue the upward trend.
The boost in enrollment is due, in part, to the enhanced subsidies, which lowered premiums to $10 or less a month for some low-income consumers, and eliminated a cutoff threshold, allowing some higher-income families to qualify for at least some subsidy, said Corlette.
Antos agreed that the administration has made changes that "clearly built on Obamacare and expanded spending and probably did cover more people."
What happened with the financial incentives meant to get states to expand their Medicaid programs to include more low-income adults, particularly those at or below the poverty level who have no children? Those incentives are still there for the taking, but, so far, no states have done so.
South Dakota expanded its Medicaid program, but that was because voters approved a ballot measure, not because of the financial incentives in the 2021 American Rescue Plan.
"That was part of Biden's goal, to close the coverage gap," said Joan Alker, executive director of the Center for Children and Families at Georgetown. "We still have 11 states resisting Medicaid expansion, and that leaves a big, gaping hole in coverage in those states. But that's not for lack of trying by the Biden administration."
Because enrollment is up, subsidies are more available, more people are helping consumers enroll, and there are additional enticements to get states to expand Medicaid, we rate this as a Promise Kept.
Telephone interview with Sabrina Corlette, co-director of the Center on Health Insurance Reforms at Georgetown University, Dec. 20, 2022
Telephone interview with Joseph Antos, senior fellow at the American Enterprise Institute, Jan. 5, 2023
Telephone interview with Joan Alker, executive director of the Center for Children and Families at Georgetown University, Jan. 10, 2023
Archive Today, transcript of Joe Biden campaign speech in Pittsburgh, Nov. 2, 2022
KHN, "Inflation Reduction Act Contains Important Cost-Saving Changes for Many Patients — Maybe for You," Aug. 12, 2022
White House, Executive Order on Continuing to Strengthen Americans' Access to Affordable, Quality Health Coverage, April 5, 2022
KFF, "Marketplace Enrollment 2014-2022," accessed Jan. 5, 2023
KFF, "Five Things to Know About the Renewal of Extra Affordable Care Act Subsidies in the Inflation Reduction Act," Aug. 11, 2022
KFF, "Navigating the Family Glitch Fix: Hurdles for Consumers with Employer-Sponsored Coverage," Nov. 21, 2022
NPR, "Shopping for ACA Health Insurance? Here's What's New This Year," Oct. 31, 2022
On March 11, President Joe Biden signed into law his first major piece of legislation, the $1.9 trillion coronavirus stimulus bill dubbed the "American Rescue Plan."
Among the many spending provisions in the bill, significant funds are earmarked for expanding health coverage through the Affordable Care Act to help many middle-income Americans who didn't previously qualify for federal subsidies or increase the subsidy amount for some who did. The measure also increased aid for low-income Americans.
These provisions represent the biggest expansion of the ACA since the sweeping health law first passed in 2010 and are Biden's first step in fulfilling his campaign promise to improve and build on ObamaCare.
"That is definitely true," said Sabrina Corlette, co-director of the Center on Health Insurance Reforms at Georgetown University. "The only revisions to the ACA that Congress has made in the last 11 years have been to chip away at it."
Subsidies, or the tax credit amount the government provides individuals to help pay for their ACA health insurance plans, are calculated based on the person's income, age and their area's average premium costs. Originally under the ACA, subsidies were only provided to those making between 100% and 400% of the federal poverty level (in 2021, that was between $12,760 and $51,040 for an individual).
The American Rescue Plan changes that calculation and sets eligibility for anyone whose marketplace plan would be more than 8.5% of their income. That is expected to increase subsidies to middle income customers.
And many people who are close to the federal poverty level who have been paying a small amount of their income to help cover their premium costs may be able to get the entire cost of their health plan covered.
The Kaiser Family Foundation estimated that these enhanced subsidies could help lower premium payments for nearly 15 million uninsured people and 14 million people insured through the individual market — though it's unclear how many will actually take advantage of the decreased premiums. The Congressional Budget Office estimated that the original House version of the bill would decrease the number of uninsured Americans by 1.3 million.
However, these additional subsidies will only be in effect through 2022, though there is the possibility that Congress could pass legislation to make the subsidy expansions permanent.
The American Rescue Plan also includes more generous financial incentives than already exist for the states — there are 12 — that didn't previously opt to pursue the ACA's expansion of Medicaid, the insurance program for low-income individuals.
Still, while the American Rescue Plan fulfills the criteria of expanding the ACA, it represents just a small part of what Democrats and Biden have said they want to do to make health insurance better and coverage affordable for all Americans.
For example, the legislation doesn't address a problem known as the family glitch, where a family is determined to be ineligible for subsidies based on an individual having access to e job-based coverage that is deemed affordable for an individual, rather than the whole family.
"As consequential as this bill is, it does not fill all the gaps that remain in our health care safety net. More work is needed to improve affordability and expand coverage," Corlette wrote in an email. "So I would expect the Biden administration will be rolling out more policies to fulfill that campaign promise, for both Congress and the executive branch."
Separate from the ACA, the covid relief law also includes subsidies for those who are unemployed and choose to extend their health coverage through COBRA — a federal program that allows recently unemployed people to purchase private insurance coverage from their former employers. This type of insurance is expensive, so the law's promise to pick up 100% of the cost of this coverage will significantly help those out of work, including people who lost their jobs as far back as March 2020.
The COBRA subsidies are also temporary — they will only be in effect for six months from April through the end of September.
We rate this promise In the Works.
Congressional Budget Office, "Cost Estimate - Reconciliation Recommendations of the House Committee on Ways and Means," Feb. 17, 2021
Email interview with Sabrina Corlette, co-director of the Center on Health Insurance Reforms at Georgetown University, March 11, 2021
Health Affairs, "The Family Glitch," Nov. 10, 2014
KFF, "Impact of Key Provisions of the House COVID-19 Relief Proposal on Marketplace Premiums," Feb. 18, 2021
KHN, "Pandemic Aid Package Includes Relief From High Premiums," March 9, 2021
The New York Times, "Pandemic Relief Bill Fulfills Biden's Promise to Expand Obamacare, for Two Years," March 8, 2021
WMFE 90.7 FM, "American Rescue Plan Includes 100% Coverage Of COBRA Health Premiums," March 10, 2021